
concomitant CIS
in RNU
specimens. Advanced pT
stage
and
positive
LVI
were
significantly
linked
to
elevation
of
preoperative
plasma
fibrinogen,
whereas
CRP
elevation
was
significantly
linked
to
positive
LVI
in
our
population.
Spearman
rank
correlations
among
continuous
variables of
three markers were
0.320
for
NLR
and
plasma
fibrinogen
(
p
<
0.001),
0.304
for
NLR
and
CRP
(
p
<
0.001),
and
0.548
for plasma
fibrinogen and CRP
(
p
<
0.001). We
found a high
positive
correlation
between
preoperative
plasma
fibrino-
gen and CRP
levels, whereas the positive correlations among
preoperative NLR,
plasma
fibrinogen,
and
CRP
levels were
only moderate.
During
follow-up
of
the
394
patients,
113
(28.7%)
experienced
disease
recurrence
and
82
(20.8%)
died
of
disease.
Figure 1shows
the
estimated
probabilities
of
recurrence-free
and
cancer-specific
survival
based
on
the
CMS.
The
risks
of
disease
recurrence
and
cancer-specific
mortality
rose
along with an
increase
in CMS
(
p
<
0.001
for
both). When
none
of
the
markers
were
elevated,
recur-
rence-free and cancer-specific survival rates were 77.2% and
84.4%,
respectively,
at
3
yr. When
all
three markers were
elevated,
recurrence-free
and
cancer-specific
survival
rates
decreased
to
48.0%
and
50.0%,
respectively,
at
3
yr.
Table 2shows
associations
of
the
CMS
with
clinicopathologic
variables.
An
increased
CMS
was
significantly
associated
with worse pathological
features, such as advanced pT stage
and
positive
LVI,
whereas
no
significant
difference
was
found
for
age,
sex,
tumor
location,
and
presence
of
CIS
among
the
four
groups.
In
addition,
patients
in
the
two
elevated
marker
groups
tended
to
have
tumor
grade
3
compared with
patients with
no
or
one
elevated marker.
Univariate and multivariate
analyses were performed
to
determine
the
predictors
of
subsequent
recurrence
and
cancer-specific
mortality
following
RNU.
Multivariate
analyses
that
included
all
three
markers
separately
indicated
that
elevations
of
NLR,
plasma
fibrinogen,
and
CRP
levels
were
associated
with
both
disease
recurrence
( Table 3)
and
cancer-specific mortality
( Table 4)
following
RNU. When
all
three markers were
included
in
one model,
only
CRP
elevation
retained
an
independent
association
with
disease
recurrence
and
cancer-specific
mortality.
Moreover,
multivariate
analysis
revealed
that
the
CMS
was
significantly
associated with
both
disease
recurrence
( Table 3)
and
cancer-specific mortality
( Table 4)
following
RNU.
Addition
of
CMS
to
a
standard
multivariate
model
improved
predictive
accuracy
by
2.7%
for
disease
recur-
rence and 3.9%
for cancer-specific mortality, which were
the
highest
among
our
prognostic models.
A
total
of
102
subjects had
died
by
the
time
of
analysis.
The Kaplan-Meier
curves
in
Supplementary
Figure S1
show
an
estimated
probability
of
overall
survival
based
on
the
CMS, demonstrating
that
the
risk of all-cause mortality
rose
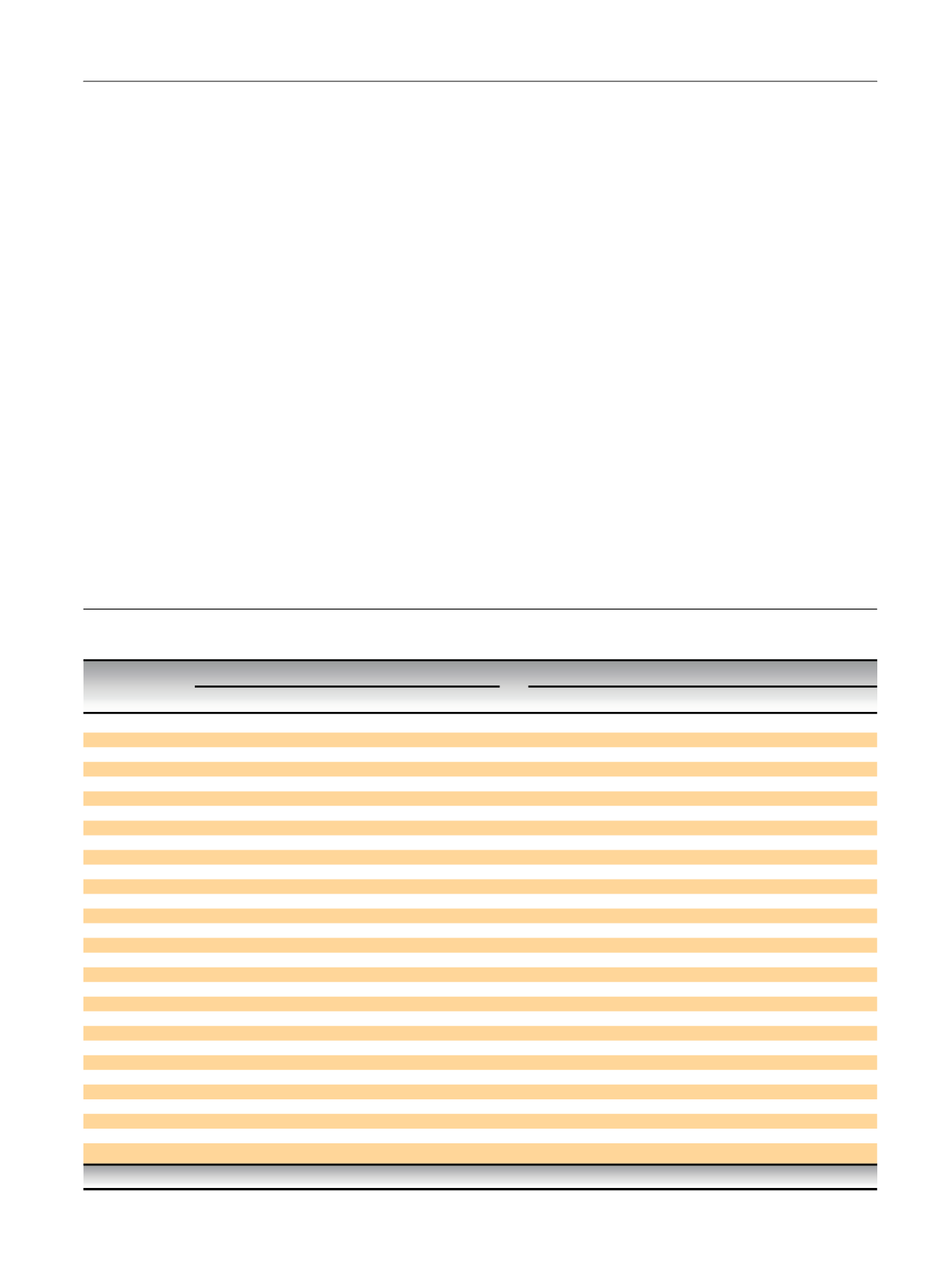
Table
2
– Association
of
baseline
clinicopathologic
characteristics
and
number
of
cumulative marker
score
in
394
patients
treated with
radical
nephroureterectomy
Cumulative marker
score,
n
(%)
p
value
Characteristic
0
(
n
= 203)
1
(
n
= 102)
2
(
n
= 52)
3
(
n
= 37)
0
vs
1
0
vs
2
0
vs
3
1
vs
2
1
vs
3
2
vs
3
Age
at
RNU
70
yr
112
(55.2)
51
(50.0)
28
(53.8)
14
(37.8)
>
70
yr
91
(44.8)
51
(50.0)
24
(46.2)
23
(62.2)
0.393
0.864
0.052
0.652
0.204
0.136
Sex
Male
149
(73.4)
78
(76.5)
36
(69.2)
26
(70.3)
Female
54
(26.6)
24
(23.5)
16
(30.8)
11
(29.7)
0.562
0.548
0.694
0.333
0.457
0.916
Tumor
location
Renal
pelvis
122
(60.1)
58
(56.9)
28
(53.8)
24
(64.9)
Ureter
81
(39.9)
44
(43.1)
24
(46.2)
13
(35.1)
0.588
0.414
0.585
0.721
0.397
0.299
Tumor
grade
G1/2
75
(36.9)
35
(34.3)
8
(15.4)
10
(27.0)
G3
128
(63.1)
67
(65.7)
44
(84.6)
27
(73.0)
0.652
0.003
0.246
0.013
0.417
0.178
Pathologic
T
stage
pTa-1
81
(39.9)
21
(20.6)
12
(23.1)
11
(29.7)
pT2
30
(14.8)
19
(18.6)
4
(7.7)
4
(10.8)
pT3
88
(43.3)
62
(60.8)
33
(63.5)
18
(48.6)
pT4
4
(2.0)
0
(0)
3
(5.8)
4
(10.8)
0.002
0.015
0.033
0.032
0.003
0.546
Lymphovascular
invasion
Negative
122
(60.1)
66
(64.7)
19
(36.5)
17
(45.9)
Positive
81
(39.9)
36
(35.3)
33
(63.5)
20
(54.1)
0.435
0.002
0.109
0.001
0.046
0.373
Concomitant
carcinoma
in
situ
Negative
162
(79.8)
87
(85.3)
39
(75.0)
32
(86.5)
Positive
41
(20.2)
15
(14.7)
13
(25.0)
5
(13.5)
0.243
0.449
0.342
0.117
0.859
0.184
Lymph
node
involvement
pNx
186
(91.6)
94
(92.2)
47
(90.4)
30
(81.1)
pN0
3
(1.5)
1
(1.0)
3
(5.8)
1
(2.7)
pN+
14
(6.9)
7
(6.9)
2
(3.8)
6
(16.2)
0.937
0.145
0.140
0.166
0.176
0.114
Adjuvant
chemotherapy
No
165
(81.3)
79
(77.5)
35
(67.3)
27
(73.0)
Yes
38
(18.7)
23
(22.5)
17
(32.7)
10
(27.0)
0.430
0.029
0.245
0.175
0.583
0.567
RNU =
radical
nephroureterectomy.
E U R O P E A N
U R O L O G Y
F O C U S
1
( 2 0 1 5
)
5 4 – 6 3
57

















