
1.
Introduction
The
prognosis
of
upper
tract
urothelial
carcinoma
(UTUC)
remains
poor
due
to
a
high
rate
of
disease
relapse
after
resection
[1–4].
Radical
nephroureterectomy
(RNU)
is
the
gold
standard
for
the
treatment
of
nonmetastatic
UTUCs;
however,
the
5-yr
disease-specific
survival
rate
is
<
50%
for
pT2–3
tumors
and
<
10%
for
pT4
tumors
[1] .To
predict
UTUC
outcomes,
many
researchers
have
attempted
to
identify
potent
biomarkers
using
human
tissue
and
blood
samples
[1,5,6], although
the vast majority of markers have
not
yet
been
applied
in
clinical
practice.
In
this
regard,
a
growing body of
evidence
suggests
the
efficacy of
systemic
inflammatory markers
from
blood
samples
for
predicting
patient
prognosis
and
pathologic
profiles
in
UTUC
[7–12],
and
these
biomarkers may
become
useful
because
of
their
low
cost
and
easy
accessibility.
The
associations
between
the
involvement
of
systemic
inflammation
and
cancer
development
are
now
evident.
Tumor
recruits endothelial cells,
fibroblasts, and
inflamma-
tory
cells
into
the
tumor
bed
and
then
shapes
its
unique
stroma,
suggesting
that
the
elevation
of
systemic
inflam-
matory
markers
may
reflect
the
development
of
an
inflammation-associated
microenvironment
in
tumors
[13–16].
In
UTUC, we
and
others
reported
the
prognostic
value of
typical preoperative
inflammatory markers
such as
neutrophil-to-lymphocyte
ratio
(NLR),
plasma
fibrinogen,
and
serum
level
of
C-reactive
protein
(CRP)
in
patients
following
RNU
[7–12].
In
the present
study, we hypothesize
that
combinations
of
these markers would
provide more
accurate
prognostic
models
than
a
single marker.
The
aim
of
this
study was
to
determine
the
associations
of
preoperative
NLR,
plasma
fibrinogen,
and
CRP with
clinicopathologic
features
and
to
develop multivariate models
for
prognosis
based
on
each
inflammatory marker
alone
or
in
combination.
2.
Patients
and methods
After
institutional
review
board
approval,
a
total
of
seven
Japanese
institutions—Keio
University
Hospital
and
six
affiliated
institutions—
provided data on 457 patients who underwent open or
laparoscopic RNU
for
localized UTUC between 1995 and 2011. We excluded patients with a
history
of
muscle-invasive
urothelial
carcinoma
(UC)
of
the
urinary
bladder
and
those
who
received
neoadjuvant
chemotherapies.
After
excluding patients without
a
full
set of blood data
and
those with
active
infection
accompanied
by
fever
(
>
38
8
C),
the
presence
of
hematological
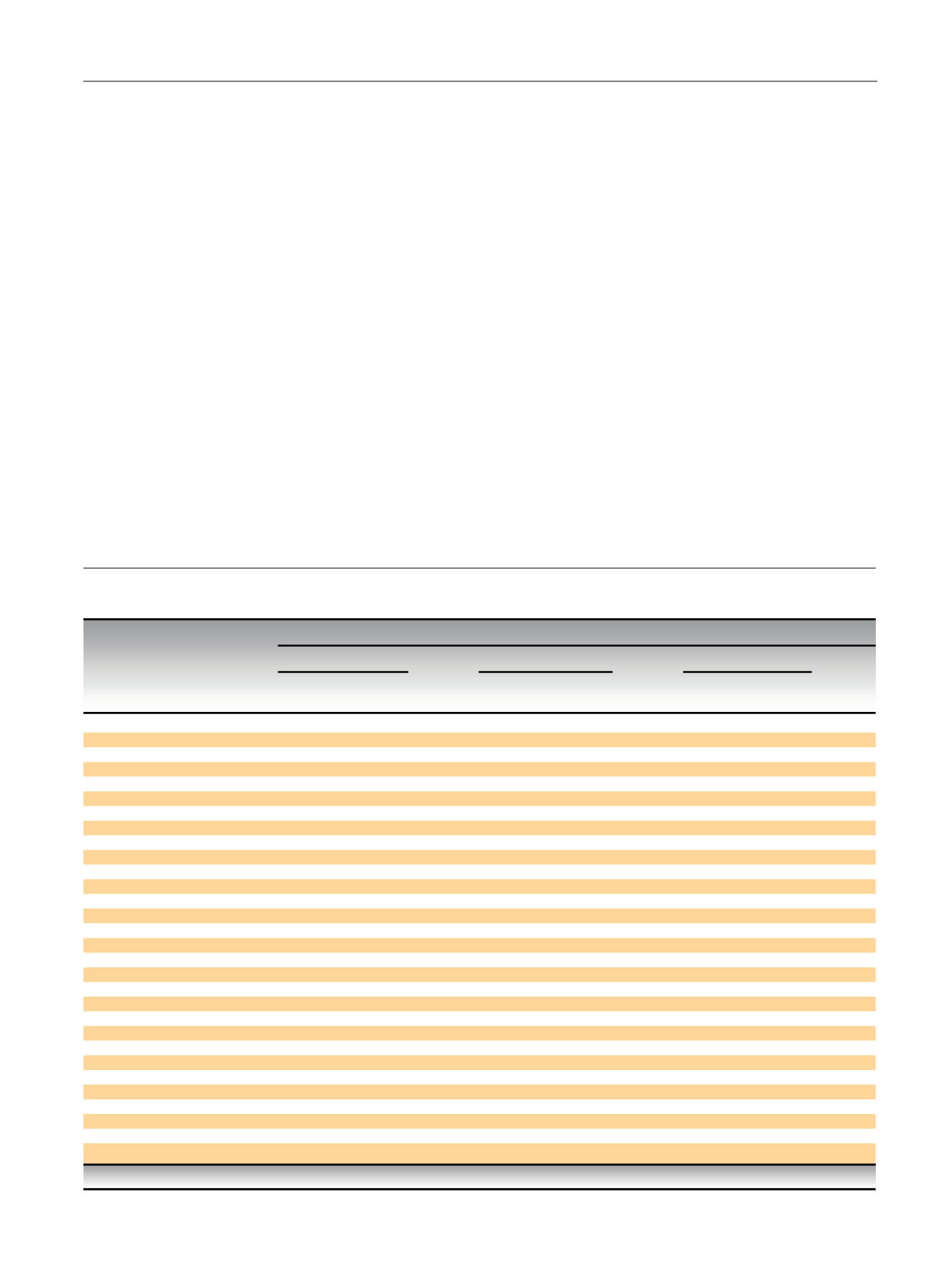
Table
1
– Association
of
baseline
clinicopathologic
characteristics
and
elevation
of
preoperative
neutrophil-to-lymphocyte
ratio,
plasma
fibrinogen,
and
serum
C-reactive
protein
in
394
patients
treated with
radical
nephroureterectomy
Elevation
of
preoperative marker
levels
NLR,
n
(%)
Plasma
fibrinogen,
n
(%)
Serum
CRP,
n
(%)
Characteristic
All
patients
(
n
= 394),
n
(%)
Elevated
(
n
= 108)
Nonelevated
(
n
= 286)
p
value
Elevated
(
n
= 117)
Nonelevated
(
n
= 277)
p
value
Elevated
(
n
= 93)
Nonelevated
(
n
= 301)
p
value
Age
at
RNU
70
yr
205
(52.0)
46
(42.6)
159
(55.6)
57
(48.7)
148
(53.4)
46
(49.5)
159
(52.8)
>
70
yr
189
(48.0)
62
(57.4)
127
(44.4)
0.021
60
(51.3)
129
(46.6)
0.392
47
(50.5)
142
(47.2)
0.571
Sex
Male
289
(73.4)
77
(71.3)
212
(74.1)
84
(71.8)
205
(74.0)
68
(73.1)
221
(73.4)
Female
105
(26.6)
31
(28.7)
74
(25.9)
0.571
33
(28.2)
72
(26.0)
0.650
25
(26.9)
80
(26.6)
0.954
Tumor
location
Renal
pelvis
232
(58.9)
64
(59.3)
168
(58.7)
70
(59.8)
162
(58.5)
53
(57.0)
179
(59.5)
Ureter
162
(41.1)
44
(40.7)
118
(41.3)
0.926
47
(40.2)
115
(41.5)
0.804
40
(43.0)
122
(40.5)
0.671
Tumor
grade
G1/2
128
(32.5)
27
(25.0)
101
(35.3)
31
(26.5)
97
(35.0)
24
(25.8)
104
(34.6)
G3
266
(67.5)
81
(75.0)
185
(64.7)
0.051
86
(73.5)
180
(65.0)
0.099
69
(74.2)
197
(65.4)
0.116
Pathologic
T
stage
pTa-1
125
(31.7)
24
(22.2)
101
(35.3)
30
(25.6)
95
(34.3)
24
(25.8)
101
(33.6)
pT2
57
(14.5)
16
(14.8)
41
(14.3)
11
(9.4)
46
(16.6)
12
(12.9)
45
(15.0)
pT3
201
(51.0)
63
(58.3)
138
(48.3)
69
(59.0)
132
(47.7)
51
(54.8)
150
(49.8)
pT4
11
(2.8)
5
(4.6)
6
(2.1)
0.055
7
(6.0)
4
(1.4)
0.005
6
(6.5)
5
(1.7)
0.052
Lymphovascular
invasion
Negative
224
(56.9)
59
(54.6)
165
(57.7)
57
(48.7)
167
(60.3)
40
(43.0)
184
(61.1)
Positive
170
(43.1)
49
(45.4)
121
(42.3)
0.584
60
(51.3)
110
(39.7)
0.034
53
(57.0)
117
(38.9)
0.002
Concomitant
carcinoma
in
situ
Negative
320
(81.2)
95
(88.0)
225
(78.7)
93
(79.5)
227
(81.9)
74
(79.6)
246
(81.7)
Positive
74
(18.8)
13
(12.0)
61
(21.3)
0.035
24
(20.5)
50
(18.1)
0.567
19
(20.4)
55
(18.3)
0.641
Lymph
node
involvement
pNx
357
(90.6)
96
(88.9)
261
(91.3)
103
(88.0)
254
(91.7)
80
(86.0)
277
(92.0)
pN0
8
(2.0)
2
(1.9)
6
(2.1)
4
(3.4)
4
(1.4)
4
(4.3)
4
(1.3)
pN+
29
(7.4)
10
(9.3)
19
(6.6)
0.670
10
(8.5)
19
(6.9)
0.364
9
(9.7)
20
(6.6)
0.119
Adjuvant
chemotherapy
No
306
(77.7)
84
(77.8)
222
(77.6)
80
(68.4)
226
(81.6)
67
(72.0)
239
(79.4)
Yes
88
(22.3)
24
(22.2)
64
(22.4)
0.974
37
(31.6)
51
(18.4)
0.004
26
(28.0)
62
(20.6)
0.136
CRP = C-reactive
protein; NLR = neutrophil-to-lymphocyte
ratio;
RNU =
radical
nephroureterectomy.
E U R O P E A N
U R O L O G Y
F O C U S
1
( 2 0 1 5
)
5 4 – 6 3
55

















