
the
effects
of
smoking
on
UCB
prognosis
in
conjunction
with
other
demographic
characteristics,
such
as
race
and
ethnicity,
other
clinical
risk
factors,
such
as
obesity
[46],
and
multimodal
therapies
including
neoadjuvant
and
adjuvant
systemic
chemotherapy
require
further
investi-
gation.
Despite
advances
in
surgical
techniques
and
improvements
in
systemic
chemotherapies,
up
to
50%
of
patients with MIBC
experience
disease
recurrence within
5
yr
after
surgery,
and
the
majority
of
these
patients
eventually
die
of
UCB
[69] .Similar
to
NMIBC,
different
decision-making
tools
have
been
developed
to
assist
clinicians
in
patient
counseling
and
estimation
of multi-
modal
treatment
success
in MIBC
[70–72], but
are
limited
by
imperfect
discrimination.
Combination
with
blood,
tissue,
and/or
urine
biomarkers
improves
these
tools
regarding
outcome
prognostication
and
patient
selection
for multimodal
therapies
[73] .A
recently published
study
on
MIBC
patients
treated
with
RC
found
that
the
combination
of
smoking
information
and
tissue
marker
status
achieved
the
highest
level
of
discrimination
and
significantly
improved
outcome
prediction
[74] .4.
Conclusions
Cigarette
smoking
is
the
best-established,
individually
modifiable
risk
factor
for
UCB
development,
although
potential relationships with other
inherent and environmen-
tal
factors
remain ambiguous.
In addition,
there
is a growing
body
of
evidence
that
smoking
negatively
affects
UCB
outcomes.
According
to
the
currently
available
literature,
smoking
status
and
cumulative
lifetime
smoking
exposure
at diagnosis and at different
times during
treatment seem
to
affect disease
recurrence, progression, and
survival. Howev-
er,
the
evidence
is
quite
heterogeneous, mainly
because
of
the
exclusively
retrospective
study
designs. While
studies
have
demonstrated
that
long-term
smoking
cessation
reduces
the
risk
of
UCB
carcinogenesis
and
improves
prognosis,
prospective
evaluation
of
this
relationship
is
lacking.
Future
research
regarding
the
effects
of
smoking
needs
to
continue
to
improve
our
understanding,
and
prospective
studies
need
to
address
currently
unanswered
questions.
Author
contributions:
Michael Rink had
full
access
to
all
the data
in
the
study
and
takes
responsibility
for
the
integrity
of
the
data
and
the
accuracy
of
the
data
analysis.
Study
concept
and
design:
Rink,
Crivelli.
Acquisition
of
data:
Crivelli,
Rink.
Analysis
and
interpretation
of
data:
Rink,
Crivelli.
Drafting
of
the manuscript:
Rink,
Crivelli.
Critical
revision
of
the manuscript
for
important
intellectual
content:
Rink,
Crivelli,
Shariat,
Chun, Messing,
Soloway.
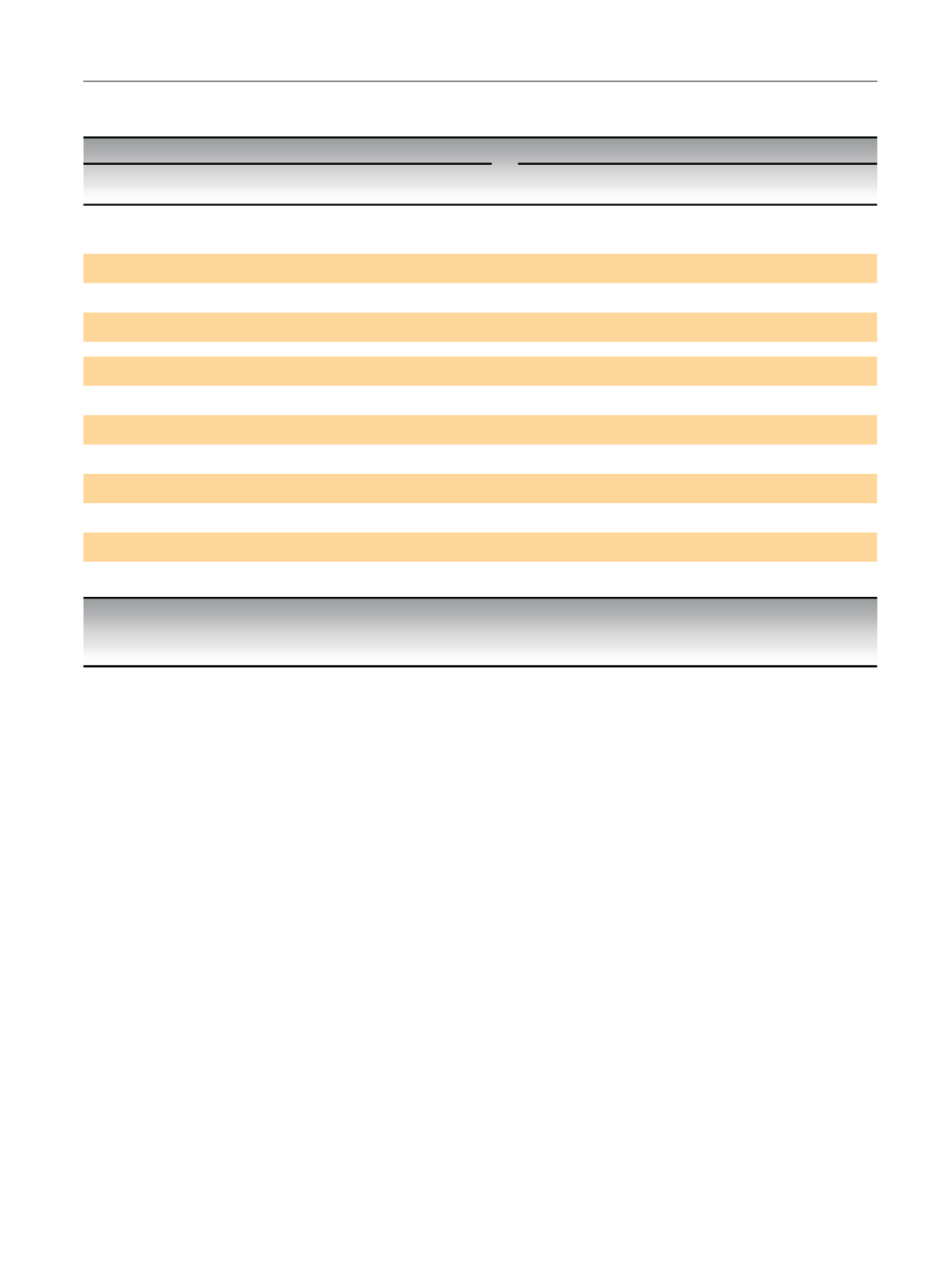
Table
4
–
Selected
studies
reporting
associations
of
smoking
cessation
and
outcomes
of
patients with
urothelial
carcinoma
of
the
bladder
treated with
transurethral
resection
of
the
bladder
or
radical
cystectomy
Selected
studies
and
their
smoking
cessation
categories
Outcomes
Intervention
Stud
y *Cessation
group
y
Comparator
group
y
Disease
Recurrence
Disease
Progression
Cancer-specific
mortality
Overall
mortality
Transurethral
resection
of
the
bladder
Fleshner
et
al.
(1999)
1-10
yr
before
1
yr
before
to
3 mo
after
HR=1.01,
p
=0.89
-
-
-
1-10
yr
before
Current
smokers
HR=0.71,
p
=0.03
-
-
-
Chen
et
al.
(2007)
>
1
yr
before
1
yr
before
to
3 mo
after
HR=1.4,
p
=0.35
-
-
-
1
yr
before
to
3 mo
after
Current
smokers
HR=0.5,
p
=0.01
-
-
-
Lammers
et
al.
(2011)
15
yr
before
<
15
yr
before
p
=0.34
-
-
-
Rink
et
al.
(2012)
10
yr
before
Current
smokers
HR=0.40,
p
<0.001
HR=0.51,
p
=0.11
-
-
<
10
yr
before
HR=1.44,
p
=0.05
HR=1.26,
p
=0.48
-
-
Rink
et
al.
(2013)
10
yr
before
Current
smokers
HR=0.66
(0.52-0.84)
HR=0.42
(0.22-0.83)
-
HR=0.98
(0.72-1.34)
<
10
yr
before
HR=1.30
(1.09-1.53)
HR=0.99
(0.65-1.50)
-
HR=1.02
(0.79-1.30)
Grotenhuis
et
al.
(2014)
10
yr
before
Current
smokers
HR=1.22
(0.88-1.68)
HR=1.40
(0.85-2.30)
-
-
<
10
yr
before
HR=1.38
(0.97-1.95)
HR=1.68
(0.92-3.07)
-
-
Radical
cystectomy
Rink
et
al.
(2013)
10
yr
before
Current
smokers
HR=0.44
(0.31-0.62)
-
HR=0.42
(0.29-0.63)
HR=0.69
(0.52-0.91)
<
10
yr
before
HR=1.08
(0.88-1.33)
-
HR=1.09
(0.86-1.37)
HR=1.05
(0.85-1.28)
HR=hazard
ratio.
Bold
:
statistically
significant
relationship.
*
Refer
to
Tables 2 and 3for
study
and
patient
characteristics.
y
Smoking
cessation
time
periods
are
relative
to
the
time
of
diagnosis.
E U R O P E A N
U R O L O G Y
F O C U S
1
( 2 0 1 5
)
1 7 – 2 7
25

















