
include
repeat
resection),
and
surveillance was
carried
out
according
to national guidelines
[9] .At
the
censor date,
the
mean
follow-up
was
106
mo
(IQR
22.0–212.8
mo)
and
1109 patients (75%) had died. The cause of death was known
for
983
patients
(89%
of
deaths;
Table 2).
3.2.
Pathological
features
There was
a
significant
association
between
tumour
stage
and death
from UBC
(
p
<
0.005,
Fig. 1). While most patients
with muscle-invasive
bladder
cancer
(MIBC)
died
from
the
disease,
the majority of patients with non– muscle-invasive
bladder
cancer
died
from
other
causes
( Table 2);
notably,
>
10%
of
patients
originally
presenting with
pTa
tumours
and
>
27%
of
patients
originally
presenting
with
pT1
tumours
subsequently
died
from UBC.
3.3.
Gender
There was no difference
in grade at presentation between the
genders
(
p
= 0.16). However,
females
presented more
com-
monly with MIBC
(30% vs 26%
for males) and
less
frequently
with
pT1
disease
(18%
vs
24%
for males;
p
= 0.06,
Table 3).
Females
had
a
longer
total
delay
time
than males
(median
120 d vs 106 d;
p
= 0.02;
Tables 3 and 4 ). The majority of
this
delay arose before hospital
referral
( Table 3 );
a
significantly
higher proportion of
female patients with visible haematuria
encountered
a
longer
delay
in
time
1
than
equivalent male
patients
(
p
<
0.05,
Table 4 ).
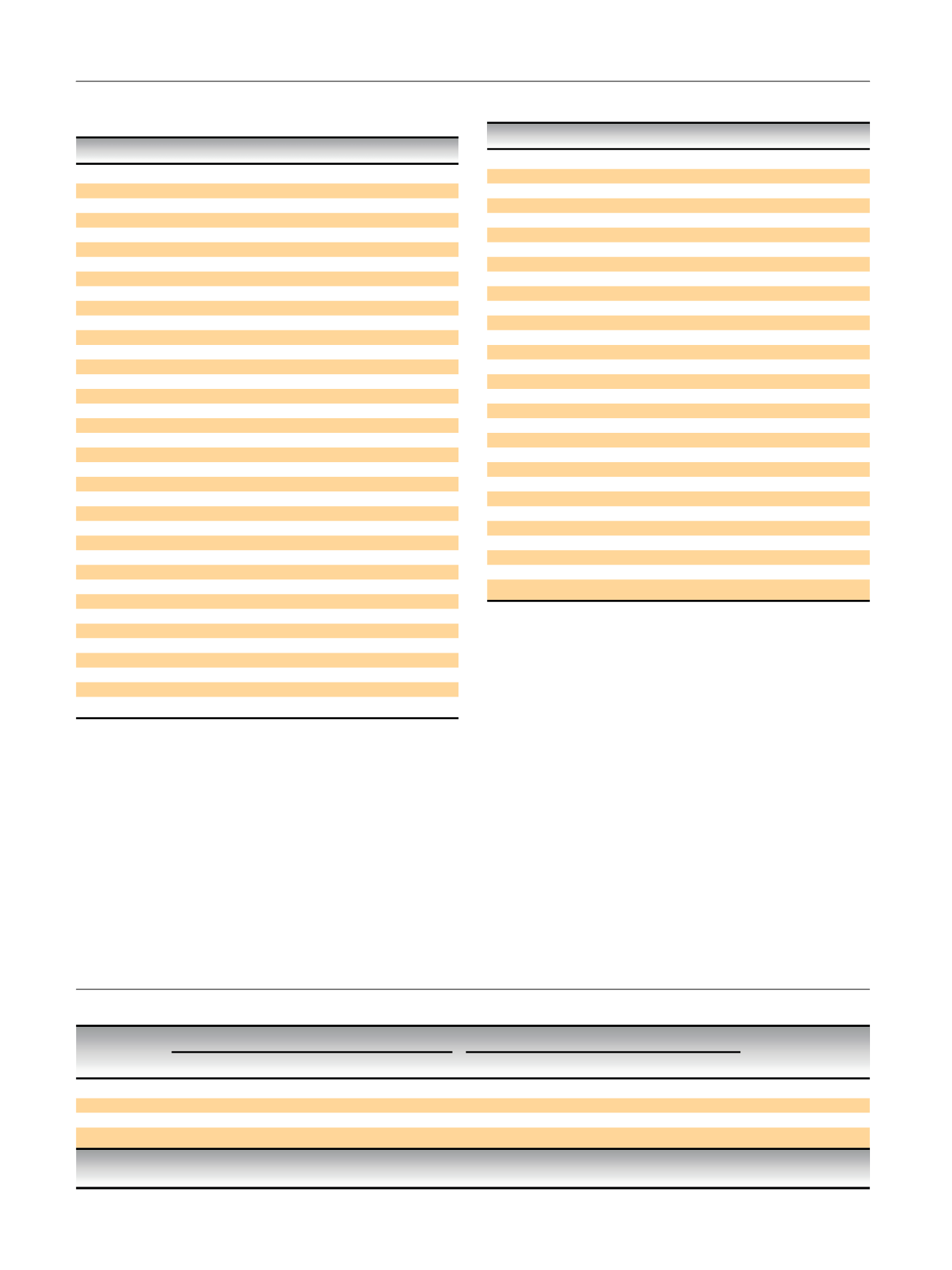
Table
1
– Overall
patient
and
tumour
characteristics
(where
recorded)
Variable
n
(%)
Gender
(1478
responses,
100%)
Male
1097
(74)
Female
381
(26)
Haematuria
at
presentation
(1171
responses,
79%)
Visible
1021
(87)
Nonvisible
67
(6)
None
83
(7)
Age
(1478
responses,
100%)
<
60
yr
315
(21)
61-70
yr
478
(32)
71-80
yr
495
(33)
>
80
yr
190
(13)
Smoking
history
(1260
responses,
85%)
Current
smoker
330
(26)
Previous
smoker
643
(51)
Never
smoked
287
(23)
Occupational
exposure
(1240
responses,
84%)
Known
or
suspected
increased
relative
risk
330
(27)
No
increased
relative
risk
910
(73)
Tumour
type
(1404
responses,
95%)
Papillary
903
(64)
Solid
246
(18)
Mixed
255
(18)
Tumour
number
(1392
responses,
94%)
Single
1042
(75)
Two
or more
350
(25)
Tumour
size
(1366
responses,
92%)
2
cm
552
(40)
>
2
cm
814
(60)
Tumour
stage
(1300
responses,
88%)
pTa
658
(51)
pT1
291
(22)
T2–T4
351
(27)
Grade
(1347
responses,
91%)
Well
differentiated
(G1)
475
(35)
Moderate
differentiation
(G2)
513
(38)
Poor
differentiation
and
anaplastic
(G3)
359
(27)
Table
2
–
Certified
causes
of
death
by
tumour
stage
for
the
983
patients
for whom
both
tumour
stage
and
cause
of
death were
known
aCause
pTa,
n
(%)
pT1,
n
(%)
T2–T4,
n
(%)
Total
G1
G2
G3
Unknown
All
grades
G1
G2
G3
Unknown
All
grades
All
grades
Bladder
cancer
31
(12)
30
(19)
5
(36)
1
(09)
67
(15)
11
(38)
39
(34)
24
(35)
5
(42)
79
(35)
219
(69)
365
Other
cancer
65
(25)
31
(20)
2
(14)
2
(18)
100
(23)
5
(17)
12
(11)
10
(14)
2
(17)
29
(13)
24
(8)
153
Other
causes
165
(63)
94
(61)
7
(50)
8
(73)
274
(62)
13
(45)
63
(55)
35
(51)
5
(42)
116
(52)
75
(24)
465
Total
261
155
14
11
441
29
114
69
12
224
318
983
G1 = well
differentiated; G2 = moderate
differentiation; G3 = poor
differentiation
and
anaplastic.
a
Rounded
proportions may
sum
to more
than
100%.
Table
3
–
Gender-specific
characteristics
of
patients
in
the
cohort
Males
Females
p
value
Patients
(%)
74
26
<
0.001
Haematuria
at
presentation
(%)
Visible
87
89
0.673
Nonvisible
6
5
None
7
6
Grade
(%)
G1
34
39
0.157
G2
39
35
G3
27
26
Stage
(%)
Ta
50
52
0.060
T1
24
18
T2–4
26
30
Median
delay
time
1
(d)
14
23
0.101
Delay
time
1
14
d
(%)
51
46
Delay
time
1
>
14
d
(%)
49
54
Median
delay
time
2
(d)
27
29
0.498
Delay
time
2
28
d
(%)
52
50
Delay
time
2
>
28
d
(%)
48
50
Median
delay
time
3
(d)
22
18
0.152
Delay
time
3
20
d
(%)
48
52
Delay
time
3
>
20
d
(%)
52
48
Median
hospital
delay
(d)
68
68
0.848
Hospital
delay
68
d
(%)
51
51
Hospital
delay
>
68
d
(%)
49
49
Median
total
delay
(d)
106
120
0.024
Total
delay
110
d
(%)
52
45
Total
delay
>
110
d
(%)
48
55
History
of
smoking
84
55
<
0.001
History
of
occupational
exposure
31
14
<
0.001
E U R O P E A N
U R O L O G Y
F O C U S
1
( 2 0 1 5
)
8 2 – 8 9
84

















