
incidence
but
showed
a
significant
11–22%
increased
risk
depending
on
the
exposure
measurement
method
(daily
amount of use,
cumulative use)
[11,61]. The data presented
by
Islami
et
al
[11]showed
a
possible
association
between
smoking
and
increased
PCa
incidence
but
only
in
studies
completed
in
1995
or
earlier, whereas
studies
completed
afterward
showed
a
null
or
even
inverse
association.
Cigarette
smoking
at
baseline
was
inversely
associated
with
incident PCa
(risk
ratio
[RR]: 0.90; 95% CI, 0.85–0.96);
however,
results
showed
high
heterogeneity
(
I
2
= 68%;
p
<
0.001).
In
meta–regression
analysis,
the
amount
of
cigarettes
smoked
per day was not
significantly
associated
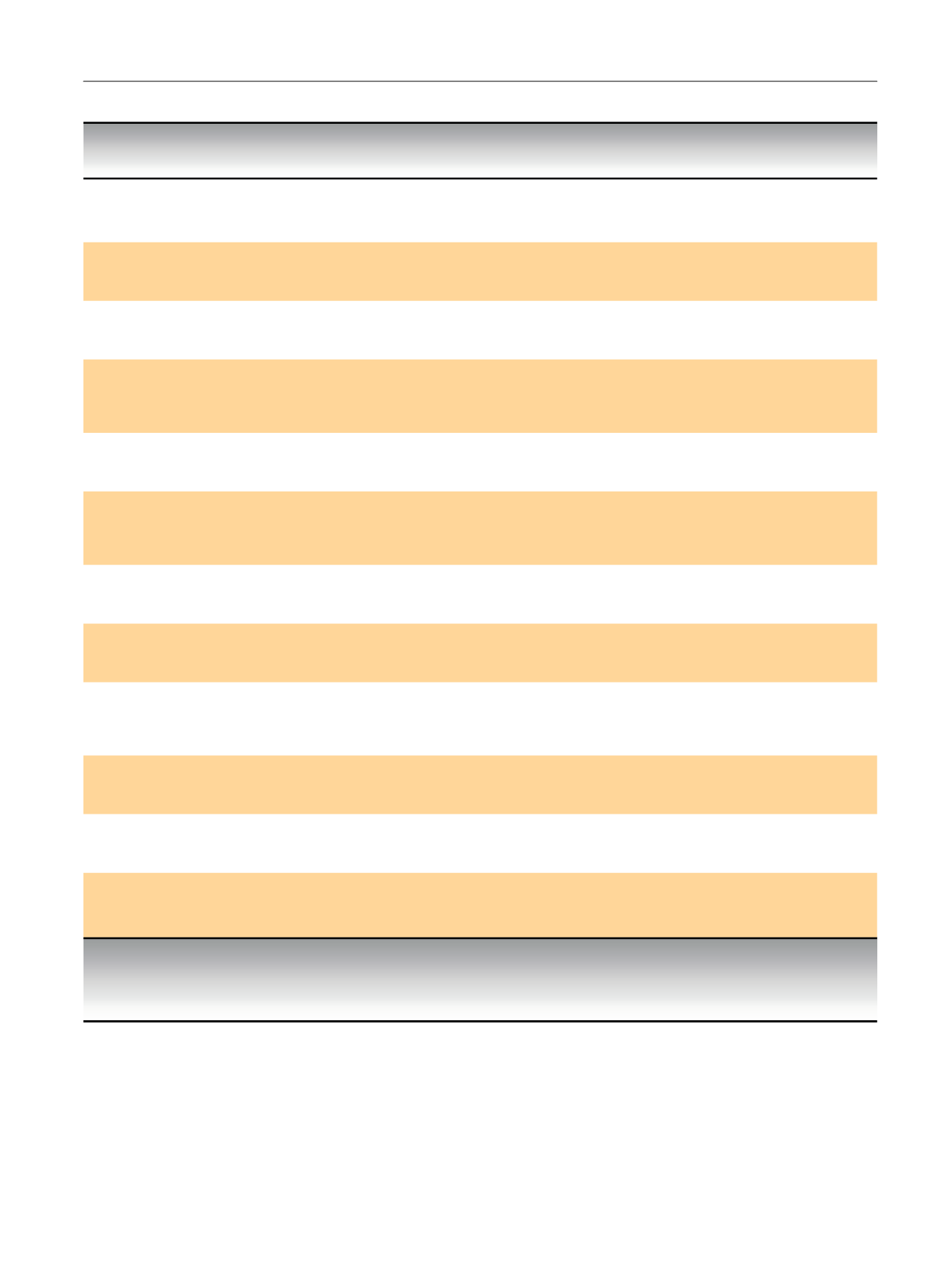
Table
2
–
Characteristics
of
studies
evaluating
the
association
between
smoking
and
prostate
cancer
treatment
outcome
Study
Study
name
(or
description);
country,
recruitment
period
Study
design,
outcome
Last
FU
(F
U a ,yr)
Total
no.
Smoking
categor
y *No.
of
case
s *Main
outcome
Roberts
et
al,
2003
[36]Johns Hopkins
RRP
series;
USA,
1992–1999
Retrospective
CCS,
RRP
1999
(NR)
1544
Never-smoker
Ever
Current
176
1157
18
Referent
1.47
(0.84–2.56)
3.17
(1.13
–
8.85)
GS
7 or pT3 disease
Pickles et al, 2004
[37]Radiation
Program,
British
Columbia
Cancer
Agency;
Canada;
1994–1997
Prospective,
CCS,
EBRT
2003
(5)
601
Never-smoker
Ever
Current
184
329
88
Referent
NR
1.68
(1.11–2.56)
PSA
relapse
Merrick
et
al,
2004
[38]USA,
1995–2000
CCS,
Brachytheraphy
2000
(54.5)
582
Never-smoker
Ever
Current
178
306
98
Reference
1.31
(NR)
2.69
(NR)
PSA
relapse
Oefelein
and
Resnick,
2004
[39]USA,
1987–2003
Retrospective
CCS
2003
(NR)
222
Never-smoker
Ever
Current
121
77
24
Reference
NR
2.7
(NR)
Castration-resistant
PCa
Panatarotto
et
al,
2007
[12]Canada,
1990–1999
Retrospective
CCS,
EBRT
1999
(NR)
434
Never-smoker
Ever
Current
120
226
70
Referent
HR:
2.90
(1.09–7.67)
HR 5.24
(1.75–15.72)
Distant
failure
Gong
et
al,
2008
[40]Seattle, WA, USA,
1993–1996
CCS,
RRP,
EBRT,
ADT
1996
(NR)
752
Never-smoker
Ever
(quit
>
10
yr)
Ever
(quit
<
10
yr)
Current
280
269
80
123
Referent
0.45
(0.19–1.05)
1.48
(0.50–
4.37)
2.66
(1.01
–
3.99)
PCa–specific
death
Kenfield
et
al,
2013
[41]The Health
Professionals
Follow–up
Study; USA,
1986–2006
Cohort
Study,
RRP,
EBRT
2008
(8.1)
5366
Never-smoker
Ever
Current
2449
2360
277
Reference
1.11
(0.96
–
1.29)
1.61
(1.16–
2.22)
PSA
relapse
Joshu
et
al,
2011
[42]Johns Hopkins
RRP
series;
USA,
1993–2006
Retrospective
CCS
2009
(7.3)
1416
Never-smoker
Ever
Current
750
571
95
Reference
1.16
(0.78–
1.74)
2.31
(1.05–
5.10)
PCa
recurrence
Dieperink
et
al,
2012
[43]Denmark,
2006–2008
Retrospective
CCS
2008
(NR)
317
Never-smoker
Ever
Current
93
175
46
Reference
NR
7.8
(NR)
EPIC
bowel
overall
bother
Oh
et
al,
2012
[44]Korea,
2004–2010
Retrospective
CCS
2010
(NR)
1165
Nonsmoker
Current
978
187
Reference
2.2
(1.04–3.83)
PSA
relapse
in
BMI
25
kg/m
2
Ngo
et
al,
2013
[45]Stanford,
CA, USA,
1989–2005
CCS,
RRP
2005
(NR)
630
Never-smoker
Current
309
321
0.031
(0.015–0.048)
Pack–yr
Cancer
Volume
Moreira
et
al,
2014
[46]Shared
Equal
Access
Regional
Cancer Hospital
(SEARCH); USA,
1995–2010
Cohort,
RRP
2010
1670
Never-smoker
Current
1121
549
Referent
2.67
(1.21–5.87)
Castration-resistant
PCa
ADT = androgen
deprivation
therapy;
BMI = body mass
index;
CCS =
case-control
study;
EBRT = external
beam
radiotherapy;
EPIC = Expanded
Prostate
Index
Composite Questionnaire;
FU =
follow-up; GS = Gleason
score;
HR = hazard
ratio; NR = not
reported;
PCa = prostate
cancer;
PSA = prostate-specific
antigen;
RRP =
radical
retropubic
prostatectomy.
*
Data
on
cigarette
smoking.
For
qualitative measures
of
use,
data
on
current
cigarette
smoking
(at
baseline)
are
shown
in
this
table.
a
The mean
or median
of
follow-up
in
years.
E U R O P E A N
U R O L O G Y
F O C U S
1
( 2 0 1 5
)
2 8 – 3 8
33

















